“…And if not now, when?” ~R. Hillel
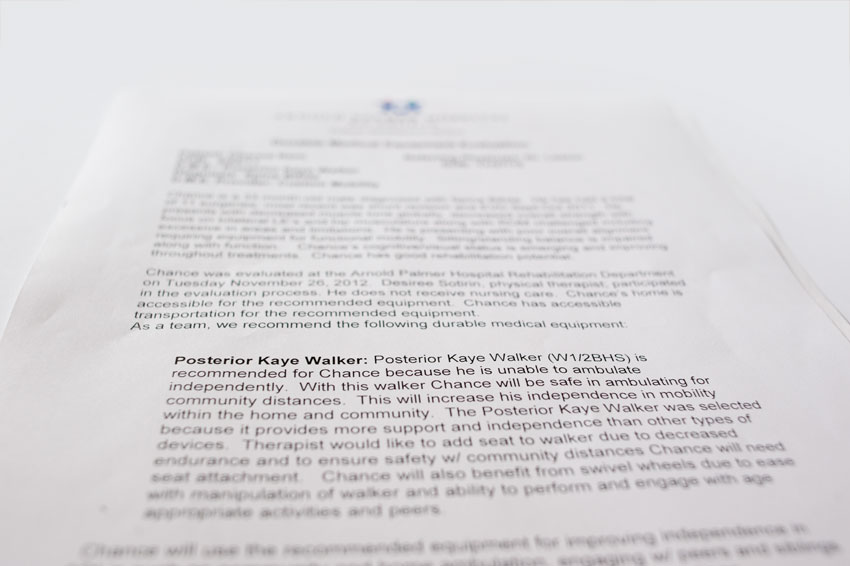
It’s been a little while since I updated my blog. I’ve been busy with quite a few things. Rather than reflecting on my busy moments (which I’m sure I’ll do soon) today is a little day that I felt it’s necessary to jot down a few thoughts after learning our current insurance company (cigna) has denied the requests for Chance’s walker. We were all in shock…our family, friends, and quite a few in the medical profession are in disbelief. How can an insurance company deny a mobility device for a child with spina bifida who clearly has needs to use the device to gain strength and hopefully become more independently mobile? This request was denied, even after his therapist and doctor spent time putting together a letter that clearly documents his needs for a walker. We were told the walker is a device of “convenience” and is not deemed to be medically necessary, even after doctors have said otherwise.
Forgive me if I’m being honest, and yes…open, about something such as this. But really this make no sense. It’s left our family and this amazing community of friends and family that’s surrounded me and my family in shock. Cigna’s denial of this request shows a significant problem with insurance. I’m sorry, a doctor goes through so much to receive their medical training if they are requesting tests, devices, etc. I surely would hope any insurance company would trust a doctor’s recommendations. This is a surprise to us all, from what I’ve been told today that this is the first time a walker has been denied locally for a child with spina bifida.
When I was pregnant with Chance I recall one of my biggest fears were the costs of raising a child with spina bifida and how we would care for a child with such significant needs and if insurance would cover his necessities. I admit as healthcare reforms change I am incredibly nervous and now I just pray insurance companies will wake up and realize that when doctors are requesting these things for patients there is a medical necessity or they wouldn’t be wasting their time requesting them. Research shared by the Spina Bifida Association on the costs of raising a child with spina bifida is incredibly outdated, from the 1980s but even this information is daunting:
“The average total lifetime cost to society for each infant born with spina bifida is approximately $532,000 per child. This estimate is only an average and for many children the total cost may be well above $1 million. Estimated annual medical care and surgical costs for persons with spina bifida in the United States exceed $200 million.”
That was in the 1980s, I’m frightened to know what that is now. In the last few years going through so much medically through the miscarriage, Chance’s pregnancy, and now all his care in his first two years of life I’ve felt incredibly blessed that we do at least have insurance because just in his first two years of life his medical expenses we’re seeing before insurances, discounts, and all that sort of stuff are far beyond the numbers shared above. Every year we, just like most families raising a child with spina bifida, max out our insurance and still pay thousands out of pocket. This walker is clearly a medical expense and should be considered as such. Sure we could go try to pay for this out of pocket, but it’d add hundreds more to the thousands we’re already paying annually if it wasn’t considered “covered” by insurance.
In speaking with the vendor we’re purchasing the walker through we’ve learned that Cigna uses two other third party companies to approve such requests. Yes, ask me why it’s taken so long for my son to get a walker…and surely the insurance approval process seems to be a big part of the delay. The vendor must go through two companies before they send the request through to Cigna and then Cigna in turn replies with their approval or in this case, disapproval. So we waited weeks for this…when someone should have been able to just contact Cigna directly to put in the request. I don’t understand, it doesn’t make sense. From a family’s point of view it surely sounds like our insurance premiums are growing higher partly because of this lack of service patients receive. Have you ever tried to contact an insurance company by phone? If you can even get through to a human being…you are often transferred many times, and many times the representatives don’t know the answers. Rather than wasting hours of my time like I have in the past I have tweeted to share my disappointment. Yes, it’s sad…but I actually receive a quicker response from my insurance company on twitter. Shortly after I sent this tweet they sent me an email to use to contact them with my concerns.

I suppose we’ll see how quickly they respond and I’m sure Chance’s doctors will do all they can to convince them otherwise. But even with taking these steps, no family should have to go through these frustrations. It’s bad enough we have a child that has all these needs…Cigna when a doctor puts in a request for a test, a device, or whatever…perhaps instead of just denying it you pick up the phone and contact the doctor directly and determine the medical necessity a little more. If Cigna representatives approving this process had any clue about spina bifida and the challenges many of the children face just getting to the point that they can walk on their own, even with a walker, perhaps they wouldn’t even second guess these sorts of requests. But no, just like most of the world…I’m sure they don’t know much about the less than 1% of the population of individuals affected by spina bifida. Cigna the patients you have covered with spina bifida need your support. If a doctor’s word isn’t enough…perhaps a video may open everyone’s eyes to just one minute of my son’s efforts to try to learn to walk with a walker…perhaps seeing it may help convince a Cigna representative that our baby boy needs this walker to help him learn to walk.
As you can see it’s hard, so very hard for him…but he’s determined and I know he will get there. I have faith in him, now I have to pray an insurance company has faith in approving something my son needs and that it doesn’t take too long to approve. In the two+ months since I shared the first photos of Chance taking steps with a walker in physical therapy I’ve watched him each week and I fear he’s begun to delay in his progress and those little legs, they’re buckling a little more. It makes me nervous still but we’ll do all we can to get him stronger. We will get him there and we have the support to know that it’s only a matter of time before he receives the support he requires, but it’s just so frustrating for our family and for so many others facing similar challenges to truly need medical care and to see it denied.
Thank you all…seriously, from the bottom of our hearts we adore you all who are out there lifting us up during the toughest moments. Jason and I have openly expressed our disappointment and so many of you have reached out to share your concern, thoughts, and offer support. I think right now we just pray Cigna is listening…we know we’re not alone in this journey and we know many families are facing the same challenges. So for now…we pray…and continue to love this little boy a little more…because surely he’s destined to show us how many amazing things he’s capable of. Surely an insurance company won’t hold Super Chance down for too long…give him time and we have faith that he’ll be walking circles around us with his walker. Don’t give up baby boy…we’ll get you there!








by Amanda Kern
2 comments